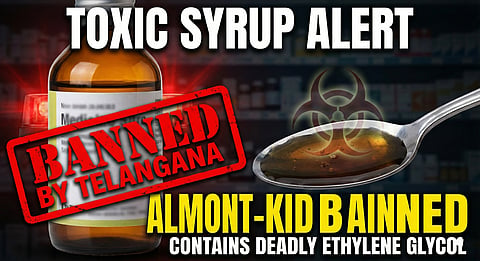
When Telangana’s Drugs Control Administration banned “Almont-Kid” syrup, it sent shockwaves across India’s pharmaceutical world. This wasn’t just about one bad batch of syrup. It tore the lid off a much bigger problem: fake and substandard medicines slipping into the market, putting lives—especially children’s—at serious risk.
Telangana's Drugs Control Administration urgently advised halting Almont-Kid Syrup use due to adulteration with toxic Ethylene Glycol. The advisory said the syrup (Batch No.: AL-24002) was manufactured by Tridus Remedies, Bihar. The syrup, often used for cough and cold symptoms in children, was found to contain Diethylene Glycol (DEG) and Ethylene Glycol (EG). These chemicals are highly toxic and can lead to severe health complications, including kidney failure and even death if consumed. The DCA has alerted all pharmacies and medical practitioners to stop the sale and distribution of this specific product immediately.
Investigators moved fast on Almont-Kid syrup after picking up intel during routine checks. The syrup, sold as a kid-friendly nutritional supplement, reportedly packed high levels of hidden, hazardous ingredients. Officials aren’t sharing all the details yet, but the risks ranged from allergies to serious organ damage. “This ban is about protecting people,” said one DCA officer, who didn’t want to be named. “We found major violations in how this syrup was made. It wasn’t safe, and it didn’t do what it promised.”
Troubling Numbers: This Isn’t a One-Off
If you think Almont-Kid is an isolated case, think again. India’s called “the pharmacy of the world,” but ironically, it fights its own battle against subpar and fake medicines. The World Health Organization says up to 10% of medicines in low and middle-income countries are substandard or outright fake. In some places, that number shoots up to 30-50%. India has strict rules on paper, but enforcing them? That’s a different story.
The government’s own surveys tell a worrying story. In a 2017-19 national study, about 3.16% of medicines on the market didn’t meet standards. That may sound small, but with India’s massive population, it means millions of doses aren’t up to scratch.
Then there’s the haunting memory of the deadly cough syrup cases in 2022 and 2023. Dozens of children died in Gambia, Uzbekistan, and Cameroon after taking Indian-made syrups tainted with toxic industrial chemicals. Those tragedies hit India’s reputation hard.
And here’s the thing: experts are convinced the real scope of the problem is much bigger. Lots of cases go unreported. Testing labs are stretched thin, many people don’t know when a drug’s gone wrong, and doctors rarely report side effects.
How Do Bad Medicines End Up on Shelves?
So, how do these dangerous products slip through? It’s a messy mix:
Not Enough Inspectors: India has over 11,000 drug factories, but not nearly enough inspectors to check them all. Some states barely have any working labs.
Profit over Safety: Some manufacturers cut corners—using cheap ingredients or skipping essential safety steps. Sometimes they swap pharmaceutical-grade chemicals for industrial ones, or mess up dosages.
Regulatory Maze: Drug regulation is split between central and state agencies. Coordination is patchy. Rules get enforced unevenly.
Easy-to-Exploit Licensing: Getting or renewing a manufacturing license isn’t as tough as it should be. Some places barely check the factories at all.
Opaque Supply Chains: Medicines pass through multiple hands before reaching the pharmacy. Tracing a bad batch back to its source is a nightmare.
Regulatory Loopholes for Supplements: Products sold as “nutraceuticals” or “health supplements” don’t always face the same checks as medicines. They can slip under the radar, and that’s a huge problem when kids are involved.
The Real-World Fallout
This isn’t just about numbers or headlines. When a child takes a tainted syrup, it can mean kidney failure, brain damage, or worse. Adults aren’t safe either—bad drugs can mean longer illness, failed treatments for diseases like TB or cancer, and a growing distrust in the healthcare system itself. People start to wonder: if medicine isn’t safe, what is?
Moving Forward: Time to Get Serious
Banning Almont-Kid is a big move, but let’s be honest, it’s just a reaction. If India really wants to tackle this problem, there’s a lot more to do. First, we need way more drug testing labs and people who know what they’re doing. Surprise inspections should be the norm, not the exception. On top of that, manufacturers turning out fake or low-quality drugs shouldn’t get off easy—real consequences matter if we want to scare off the bad actors. Tech can help too. If every medicine came with a QR code or got logged through block-chain, tracking it from the factory to the pharmacy would be so much easier. People could spot fakes, and so could the authorities. But you can’t leave everything to regulators. Public awareness matters. People need to know how to spot real medicines and where to report anything fishy. And regulators themselves need to get on the same page—central and state agencies should actually work together, with clear and consistent rules.
Then there are the basics - every manufacturing unit has to stick to Good Manufacturing Practices. Regular audits shouldn’t just be a box to tick—they should really mean something.
The Telangana DCA’s crackdown is a wake-up call. India might be proud of its pharma industry, but keeping people safe is a never-ending job. The threat of substandard drugs isn’t going away, and it’s time for real, constant action—not just one-off bans.
